Measles comes to Kentucky: experts discuss what’s next
Do state's declining vaccination rates mean greater risk of contagion?

Earlier this week, state and Franklin County public health officials announced Kentucky’s first case of measles in 2025.
The Frankfort resident was identified as having been infected with the highly contagious virus after traveling abroad where an outbreak of measles was occurring. The state is now making an effort to locate anyone who might have come into contact with this person, according to a statement.
“Measles is one of the most contagious viruses in the world,” Kentucky Department of Public Health Commissioner Dr. Steven Stack, said in the statement. “Fortunately, measles can be prevented with the measles, mumps and rubella (MMR) vaccine, which is safe and effective.”
The measles virus, when airborne, can survive for up to two hours after an infected person leaves an area. A person can be infected and still be asymptomatic for between 8-12 days after exposure. Symptoms include high fever, cough, runny nose and red and or watery eyes. A rash typically appears three to five days after symptoms begin, typically on the inside of the cheek and on the face, then spreads across the body.
Call ahead
The commissioner warned that if you need to see a healthcare practitioner because you suspect you or a loved-one has the measles, be sure to call ahead. “Make them aware of your measles exposure and symptoms prior to entering so that others are not exposed,” added Dr. Stack.
Telemedicine is another option, according to a Lexington internist specializing in pediatrics.
“We may have to start seeing patients in a telehealth visit to avoid any contamination,” Alexander Hernandez, MD, a CHI Saint Joseph Medical Group primary care physician in Lexington, told The Edge. “That is not optimal because we also can’t do an exam to see what’s causing the fever, or do a lung exam to see if there is anything wrong with the lungs,” Hernandez said in a phone interview.
Hernandez said due to the reported case in Frankfort, he plans to work with his patient call center to help them screen patients for measles in order to help avoid infecting others in his waiting room.
Tell-tale signs of measles
Because of its rarity, not all physicians will have encountered measles in their practice, according to Hernandez. The most classic presentation of measles is the rash, he said. “It's not 100% that you will see the spots, or maybe the person is presenting after the spots have resolved, but typically there are a couple spots in the mouth and the gums,” he said. “They will be whitish-gray, the spots on the cheeks inside the mouth, and there's some surrounding redness around that white spot. It can sometimes involve the lips as well, then it spreads down the body to the soles of the feet.”
After the rash disappears, Hernandez said a person is still infectious for at least another five days.
Usually, it will be the fever that tips off the primary care clinician to think measles in the current environment, according to Hernandez.
“I always ask patients if they have been exposed to anyone who was sick, and if so, whether they know what the person had,” Hernandez said. “That can help us be more suspicious of whether it’s measles, because if you don’t present with the typical symptoms, it could sound like any other viral respiratory infection, but there can be drastic long-term outcomes if you don’t address it and it turns out to be measles.”
Vaccination recommendations
Hernandez says most of the patients he sees have been requesting information about the MMR schedule, and have been proactive about keeping themselves and their family up to date on their shots.
He recommends that anyone born between 1964-1968 should be re-vaccinated, because the vaccine at that time was ineffective and caused adverse outcomes for some people. Persons vaccinated post 1968 should be okay, Hernandez said.
For persons born prior to 1957, Wooton said they are naturally immune because measles were common back then. Otherwise, she said, “Check your status. That’s one way to stop the spread. If you’ve had two doses as an adult, you’re good,” she said.
One exception Hernandez noted was that it is better to wait for an MMR dose if a person has had a different live vaccine shot in the past month.
Infants less than a year old are ineligible for the vaccine and must be protected as much as possible from possible infection, Hernandez said.
Vaccinations decline post-pandemic
Increasingly, however, Kentuckians are rejecting vaccination of their children. The state has seen vaccination rates trend downward in recent years. During the 2023-2024 school year, 90% of Kentucky kindergartners reportedly received the MMR vaccine, according to the Centers for Disease Control and Prevention. That was down from just over 93% of Kentucky kindergarteners having been immunized in the 2019-2020 school year.
Nationally, vaccine rates in children are also down. Currently the rate for all reported vaccines is 92.7%, down slightly from 93.1% in 2022-2023, according to the CDC. Similar trends have continued for DTaP (diphtheria, tetanus and pertussis) and polio vaccines since the pandemic, the data show.
The CDC's stated target for all vaccines is a rate of 95%, which it says is the threshold necessary to thwart community outbreaks of infectious diseases.
‘Mistrust of science’
As to why vaccination rates are declining, The Edge spoke with an expert in Texas where the first measles outbreaks this year were reported. Public health officials there released a media advisory earlier this week, reporting there were at least 124 cases of measles in the state, primarily in West Texas, where a school-aged child died after testing positive for the virus on Tuesday.
“I think after COVID, people are more wary, they are less trustful of science,” Susan H. Wooton, MD, a professor of medicine, and a pediatric infectious disease specialist at McGovern Medical School at the Texas Medical Center in Houston, told The Edge in a phone interview.
“We've always had an anti-vaccine movement for as long as we've had vaccines. But with social media the capacity to spread vaccine disinformation is exponential,” Wooton said. “For whatever reason, the people who won’t vaccinate feel the risks outweigh the benefits.”
Current federal views
The Trump administrations’ secretary for Health and Human Services, Robert F. Kennedy, Jr., is an outspoken opponent of vaccinations. Last week, the RFK, Jr.-founded Children’s Health Defense released an article pushing back on his critics and arguing that slipping levels of herd immunity is not what causes outbreaks, ineffective vaccines do.
“For over 25 years, [measles] outbreaks have been reported in populations with vaccination rates exceeding 95%, undermining the mainstream assumption that vaccines are the singular solution to measles control,” read the piece, citing multiple journals that published evidence to that effect from 30 or more years ago.
In the administration’s first cabinet meeting held earlier this week, Kennedy noted that the measles in Texas are primarily in Mennonite communities and said, “It’s not unusual. We have measles outbreaks every year.”
Federal data largely support this assertion, although outbreaks in the US tend to be small and contained, unlike the situation currently in Texas, according to the CDC.
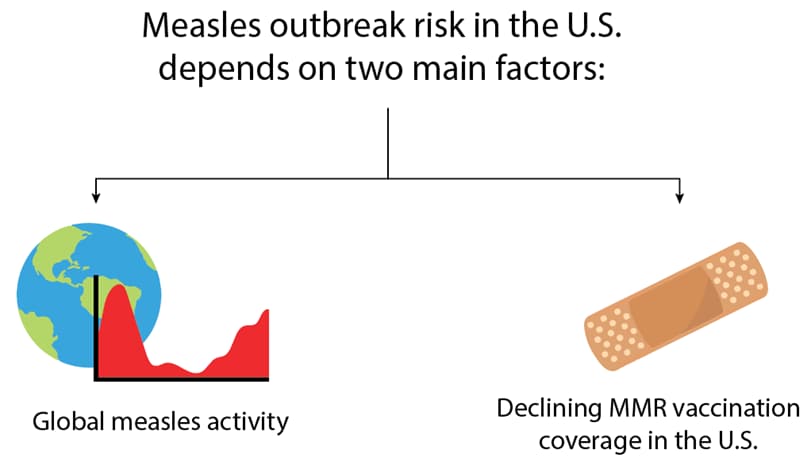
In contrast to the Children’s Health Defense claims about what causes outbreaks, the CDC has a graphic on its website specifying the two reasons for mass contagion when it occurs in the US are global importation and lowering vaccination rates.
Eliminated, not eradicated
The US declared measles eliminated in 2000, meaning that there have been no sustained transmissions of the virus for more than 12 consecutive months, according to Wooton. To have been eradicated would have meant measles no longer exist.
Texas and New Mexico currently have the largest outbreaks so far this year. Other US locations, in addition to Kentucky, where cases have been reported as of today, February 28, include Alaska, California, Georgia, New Jersey, New York City, and Rhode Island.
The last case of measles detected in Kentucky occurred in February 2023, according to the public health department’s statement.
Globally, measles are on the rise. The World Health Organization and UNICEF jointly reported in 2022 that cases of measles around the world had increased by 79% in the first two months over the same period in the previous year, citing lack of access to vaccines as the primary cause.
To date, Secretary Kennedy’s office has not released any federal media advisories about the current measles outbreaks, although the CDC, which is under the authority of the HHS, has.
What might come in Kentucky
Hernandez said that even though state vaccination rates are lower than the CDC target rate, he hopes the current case in Frankfort will remain isolated, and if not, that the virus won’t spread too far. “I hope our 90% immunization rate is enough to prevent things from becoming chaotic.
The Edge is Berea’s source for reliable, rigorous journalism. Please support it with your paid subscription.

